Health + Medicine
Feature
Restoring Quality of Life at Hadassah’s Rehab Department

Salwa Abed Rabu, a 58-year-old journalist from East Jerusalem, shuffles forward, balancing on two sturdy canes, her feet propelling a large ball with each step. Disabled by three severe strokes that caused weakness on both sides of her body and loss of balance, she has been coming to the Department of Physical Medicine and Rehabilitation at Hadassah Medical Organization’s Mount Scopus campus three times a week for the past year. She has regained 70 percent of functioning and is working hard to get back the remainder.
Terror victim Aluma Mekaitan Guertzenstein spent six years in rehab at Hadassah beginning at age 17, after a suicide bomber boarded the bus she rode to school on November 21, 2002. Over 30 pieces of shrapnel ripped through her right arm and leg, but it was the rusty half-inch metal fragment that pierced her brain that did the major damage. While she has largely recovered speech and mobility, she has foot drop in her right leg, and her right hand is paralyzed. Now 34, she recently gave birth to her first child after having returned to Hadassah during her pregnancy where she learned strategies to help her care for her soon-to-be-born baby.
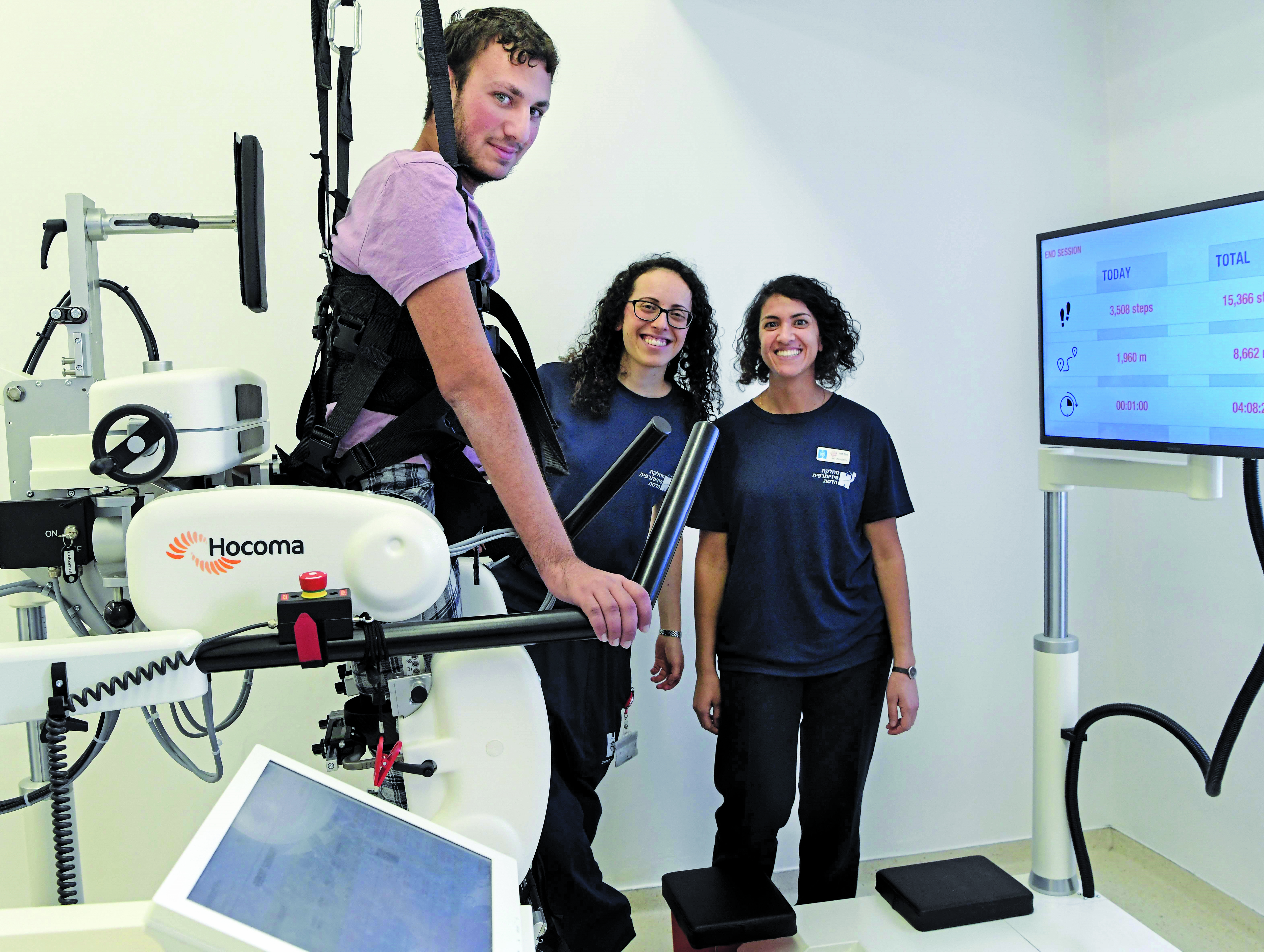
Former Israel Defense Forces combat soldier Dvir Teitelbaum, 21, tirelessly paces on Hadassah’s new Lokomat treadmill, paralyzed legs moved by electric motors outfitted with sensors. He has Guillain-Barre syndrome, a rare neurological disorder whose sudden onset came while he was serving on Israel’s northern border.
The progress of all three individuals delights Dr. Isabella Schwartz, 52, head of Hadassah’s rehabilitation department—as does that of the hundreds more treated in the department each week. “Rehabilitation is a supremely optimistic field,” she said. “It’s about well-being and quality of life. In restoring the ability to function to patients, you restore their will to live. I remember a 20-year-old whose bike accident had left him paralyzed, without even sphincter control. He reproached us: ‘You doctors saved my life, but it’s not a life I want to live.’ ” The department ultimately helped that young man to walk again as well as to regain control of other body functions.
When healing is complete, the department also helps patients learn to live and cope with their disabilities. All its patients come back for routine follow-up, or, like Guertzenstein, to learn a new skill. “We follow our patients forever,” said Dr. Schwartz. “They will always need us.”

Hadassah’s rehabilitation department opened on the Mount Scopus campus in 1976. A new facility, also at Mount Scopus, is now under construction, in an initiative led by Hadassah International. “I started my residency in the department in 1995, two years after my aliyah from Russia,” Dr. Schwartz recounted. “I fell in love with the possibilities of rehab, its ongoing search for new solutions.”
Today, she heads Hadassah’s rehab team of 100 physicians and nurses; occupational, physical and speech therapists; and dietitians, psychologists and social workers. Each week, she oversees treatment of the department’s 38 inpatients, 100 outpatients and hundreds more who attend the department’s specialized clinics—for post-polio syndrome, which she runs herself, along with those for gait issues, prosthetic devices, speech difficulty, neurological problems and more.
“Whereas a decade or two ago, Hadassah’s rehab patients were predominantly orthopedic, today, some 70 percent are here for neurological problems because more people are surviving stroke, brain, spinal cord and nervous system injuries, which can leave them with severe complications,” she explained.
The remaining 30 percent suffer from multiple traumas, are victims of terror, road accidents or falls, or have musculoskeletal and spinal pain syndromes, joint problems, osteoporosis complications or cardiac issues. Around 10 percent are amputees—diabetics or military or civilian casualties. And ages range from mid-teens to over 100.
“Last year, a 110-year-old man came to us after surgery on a fractured femur,” Dr. Schwartz said. “He walked out on his own two feet!”
This elderly man—like every patient treated in the department—was evaluated by all disciplines on the team to determine whether he could be helped. “We consider: What level can he reach? Is he motivated? Can he cooperate?” said Dr. Schwartz, “so that we know how to best help” the patient.
Guertzenstein, the terror victim, was hospitalized at Ein Kerem last November for minor complications during her 36th week of pregnancy. She took advantage of her stay to learn how to hold, nurse, diaper, clothe and bathe a baby with only one functioning hand. “Life is good!” she said at the time, her large brown eyes shining, a T-shirt reading “This is love!” stretched across her belly. “I have two legs, two hands—one of which even works! I’ll do whatever I have to do. I’ll never ask: ‘Can we stop now?’ I’ll always want to do more so I can take care of my baby.”
“We’ll get you there,” occupational therapist Yifat Yoniso reassured her. “We’ll practice, and we’ll find the ways.” After Guertzenstein’s baby boy, Eitan Iri, was born at Hadassah’s Ein Kerem campus in late November, she received additional occupational therapy to help her put those strategies into practice.
Yoniso, 39, has been at Hadassah for 14 years. She is one of 30 occupational therapists in the department whose job is to help patients adapt to their changed situation and promote the daily tasks of independent living, called Instrumental Activities of Daily Living (IADL) in the jargon of the specialty.
“Our work is cooperative and focused on what the patient wants,” Yoniso explained. “For this, I must get to know Aluma. Her unsteady gait and one functioning hand are only part of the picture. To help her, I must also understand her personal, family and social worlds.” And, she added, “I must never forget her immense trauma—the bus bombing that killed 11 fellow passengers, injured 50 and left her unconscious for days.”
Like the occupational therapists, Hadassah’s physical therapists largely work one-on-one with their patients, not only because their work is hands-on, but because no two treatment programs are alike—even when the medical reports are identical. “Rehab is about far more than the physical exam and the scan,” said Naama Karniel, 37, who heads Hadassah’s 40 physical therapists. “In physiotherapy, it’s about seeing who the patient is, before injury and afterward, and how hard they’re prepared to work for recovery.”
Physical therapy’s goals are always functional, she noted. “Turning in bed, sitting, standing, sphincter control, dressing, grooming, oral care, eating, climbing stairs—each is a complex task that demands fine motor skills and memory. We divide them into subtasks, use orthotic devices as necessary—a brace, for example, to stabilize or improve alignment—and practice, practice, practice, week after week, building on each advance to return our patients to their prior status, so they can work, shop, cook, live.”
Indeed, this is the goal of Abed Rabu, the journalist and multiple stroke victim. “I want to be well to care for myself and my family, to continue with my life and career,” she said. “I’ll do whatever it takes. Just months ago, I had no balance, no strength. Today, I walk, even though it’s with support, and can mostly care for myself. I plan to speak to other women felled by stroke and encourage them to work hard at recovery.”

The tools the physical therapists use range from low-tech grabbers and balls to a hydrotherapeutic pool, robotics and virtual reality. For Teitelbaum, the former soldier, the Lokomat robotic walking system has been transformative.
“I already have movement in my feet and hands,” he said, and his doctors are hopeful he will make a full recovery. “There’s still a way to go, but I celebrate every step!”
One of only 300 hospitals worldwide with a Lokomat, Hadassah was the first to bring it to Israel, in 2001, and has recently acquired a new, state-of the-art model. The Lokomat can reverse “learned nonuse” in muscles, Karniel said, the repetitive walking pattern helping the brain and spinal cord reroute damaged neural signals. Patients are strapped into a harness suspended over a treadmill and attached to robotic sensors that move their legs in a natural walking pattern. “We control how fast he walks,” explained Karniel, “how much body weight he carries and how much help the robotic legs provide.”
Leg injuries, such as torn ligaments, require a different technology, the anti-gravity treadmill. Developed in the United States by NASA, the machine encases its user from the waist down in a vacuum-sealed plastic membrane that is pumped full of air and then pressurized to absorb up to 80 percent of body weight. Unburdened, the leg muscles can be used, and thus regain their strength without pain or further injury.
“We take our ability to walk for granted,” said Dr. Tamar Elram, director of the Mount Scopus campus, “until we lose it and, with it, our independence.”
“Our aim is restoring patients to their pre-existing level of functioning,” said Dr. Schwartz. “Where this isn’t possible, we give them strategies to compensate.”
Wendy Elliman is a British-born science writer who has lived in Israel for more than four decades.










 Facebook
Facebook Instagram
Instagram Twitter
Twitter
Leave a Reply