Health + Medicine
Feature
Israel Is a Testing Ground for Treating Ovarian Cancer
Rosalyn Schofield would have dismissed the dull, intermittent ache between her hips had she not been leaving on a long-awaited trip to the Galapagos Islands. “I didn’t want to find myself sick out there,” said the 59-year-old attorney, “so I got checked—and learned I had ovarian cancer.”
Dr. Rivka Brooks, 52, was hiking in Georgia’s Caucasus Mountains when she got her period. Noting that it was different than usual, she was immediately suspicious.
“I’m not hysterical, but I think I’ve got cancer,” she messaged her Hadassah Medical Organization colleague and friend, Dr. Drorit Hochner, who heads the obstetrics and gynecology department at Hadassah Hospital Mount Scopus.
Both women are alive and cancer-free today because the disease, known for its stealthy arrival, gave them warning.
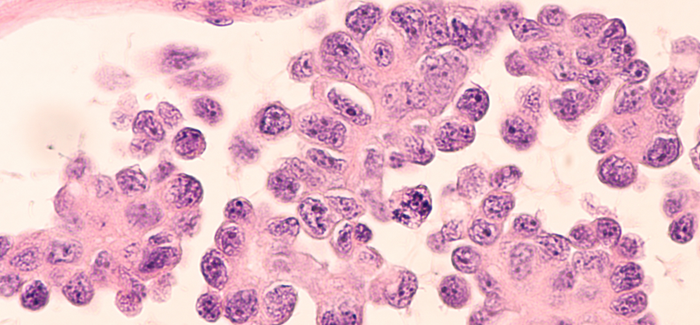
“Ovarian cancer is usually asymptomatic and goes undetected until disease is advanced,” said HMO gynecologist-oncologist Dr. Tamar Perri. “Discovered in its early stages, before it spreads, its cure rate is 95 percent. After it metastasizes, however, it turns into what was, until recently, a death sentence.”
Dr. Perri is an expert in gynecological cancers. She came to Hadassah in January 2021 to establish and run the Gynecologic Oncology Center. A facility within the Patricia and Russell Fleischman Center for Women’s Health at Hadassah Ein Kerem, the oncology center brings under one roof the treatment and follow-up of gynecological cancers—ovarian, cervical, uterine and vaginal—along with that of endometriosis, fibroids, pelvic masses and more. This approach enables swift management of conditions in which timing is often critical.

“I got back to Israel on a Friday in late June 2021 and saw Dr. Hochner on Sunday,” said the British-born Dr. Brooks, who has lived in Israel since age 3. Today, she heads the pediatrics department at Hadassah Mount Scopus. “She referred me to Dr. Perri, who diagnosed me on Tuesday. I was in surgery by Thursday and started chemotherapy two weeks later.”
Drs. Brooks and Perri discussed their patient-doctor link as well as their practices at a dinner for major donors at Hadassah’s 100th Convention in Jerusalem in November.
For most ovarian cancer patients, unfortunately, their diagnosis is not as simple as that of Dr. Brooks. One 34-year-old woman who prefers to remain anonymous experienced coughing, fever and shortness of breath that repeatedly sent her to the emergency room just as Covid-19 was tightening its grip in 2020. Testing negative for coronavirus each time—the medical staff thought she had a different virus—she would return home, only for the symptoms to persist.
She was eventually diagnosed with malignant pleural effusion, a build-up of excess fluid between the cushioning layers of pleura around her lungs.
“This often indicates advanced ovarian cancer,” said Dr. Perri. “Almost half the women who die from the disease have pleural metastases.”
In 2021, the woman became the first patient to be treated in the newly opened Gynecologic Oncology Center. Because her ovarian cancer had reached stage 4, she received three cycles of neoadjuvant chemotherapy to shrink her tumors so that eventual surgery would be less invasive and more effective. More chemotherapy followed the surgery, and the woman is now in remission.
Hadassah On Call, Hadassah’s premier podcast, helps decode today’s top developments in medicine, from new treatments to tips for staying healthy. In each episode, journalist Maayan Hoffman, a third-generation Hadassah member, interviews one of the Hadassah Medical Organization’s top doctors, nurses or medical innovators. In 2023, she’ll zero in on heart health, nutrition, new Covid-19 variants and more.
Look for past episodes on topics from women’s mental health to relief for those with sleep disorders. Subscribe and share your comments here or wherever you listen to podcasts.
While chemotherapy is not easy for anyone, the recent experience of a 43-year-old woman who struggled with infertility (she also prefers to remain anonymous) had an added dimension of concern.
“She had been in fertility treatment for eight years at the time of her diagnosis,” said Dr. Perri. “A scan seven weeks after her latest in vitro fertilization cycle finally showed a fetus—but also particularly aggressive stage 4 ovarian cancer.”
Although the cancer did not affect the growing fetus, the woman’s survival was at risk. Her medical team advised terminating the pregnancy and immediately treating the cancer. The woman, however, refused to terminate.
“She began chemotherapy at 13 weeks’ gestation, when risk of miscarriage or serious deformities to the fetus drops, although it doesn’t disappear,” said Dr. Perri. While she suffered some of the usual side effects of chemo—loss of appetite, nausea, vomiting, low blood count, bruising and infections—“the pregnancy held,” Dr. Perri recounted.
At 33 weeks, a healthy little girl was delivered by Cesarean section.
“The new mother heard her daughter cry and stroked her head,” Dr. Perri recalled. “Then we administered a full anesthetic and removed her ovaries and uterus.”
Dr. Brooks and Schofield, and the two other women described, all carry a mutation of the BRCA gene, the only proven risk factor for ovarian cancer. Those with mutations of the BRCA1 or BRCA2 genes have about a 70 percent chance of developing breast cancer and a 44 percent chance of ovarian cancer by the age of 80, according to the United States’ National Cancer Institute.
Schofield, whose mother and grandmother died from breast cancer at relatively young ages, knew there was a strong possibility of the mutation in her family, “but, I’m ashamed to say, I was too afraid to test.”
The other three, however, were astonished to learn they carried the culprit mutation.
“I couldn’t believe I was BRCA-positive!” said Dr. Brooks, who was tested after her diagnosis. “I come from a large family with no known history of cancer.”
In the general population, where the prevalence of a BRCA mutation is 0.24 percent, ovarian cancer affects one in 78—making it the fifth-deadliest malignancy in women.
“BRCA’s incidence in Ashkenazi Jewish women, however, leaps to 2.5 percent, meaning it’s carried by one in every 40,” explained Dr. Perri. “So the message is: If you’re Ashkenazi and toward your 40s, test for BRCA.”
Because of these genetic realities, Israel proportionally has one of the world’s largest populations of women with ovarian cancer, making the country a testing ground for diagnostic and therapeutic trials. One life-saving development already in wide use is BRCA inhibitors, a class of cancer-fighting drugs.

“BRCA1 and BRCA2 genes help healthy cells repair themselves,” said Dr. Perri. “When there’s a fault in one or both these genes, this ability is damaged and cancer cells can invade. Inhibitors that block a cell enzyme, called PARP, prevent cancer cells from thriving and replicating and reduce the risk of a recurrence of BRCA-associated ovarian cancer by up to 70 percent.
“PARP treatment is enabling the survival of even those diagnosed with stage 4 ovarian cancer,” she added. “I have patients like this who are alive and well six and seven years since diagnosis.”
Another direction showing promise is immunotherapy, which treats ovarian cancer by activating the natural immune system against tumor cells. While still experimental, several clinical trials are underway, and researchers are optimistic.
With cure rates high when the disease is found early, a key emphasis in research is early detection.
“Only one in five ovarian tumors is found before it spreads,” said Dr. Perri. “We at Hadassah are trying to develop a form of Pap smear in which changes in cells swabbed from the cervix will warn of ovarian cancers, as they now signal cervical malignancy.”
Until research routs gynecological cancers for good, the Gynecologic Oncology Center is easing the path for the hundreds of women who come to Hadassah each year.
“Our center is built with the patient and her family as the focus,” said Dr. Perri. “Instead of making ill, frightened women trail from one department to another for diagnosis, treatment and follow-up, everything is in one place. Alongside that, we build personal relationships with every patient, which foster better, more comprehensive care—whether it’s advanced therapy or surgery, preserving fertility or minimizing side effects, or simply giving a smile or hug at the right time.”
Wendy Elliman is a British-born science writer who has lived in Israel for more than four decades.










 Facebook
Facebook Instagram
Instagram Twitter
Twitter
Sylvia Hyman says
I’m 78 being treated for stage four ovarian cancer, is there any hope for me as far as procedures developed recently?