Health + Medicine
Feature
Using Robots in the Operating Room
Combine medieval stories of miraculous healing of the sick with the banks of monitors, sensors and technological know-how in use at the Hadassah Medical Organization in Jerusalem, and what do you get? The cutting-edge operating room of today.
First, the tales of miracles: A 21-year-old construction worker falls from a ladder and breaks his back. He spends 15 minutes in surgery at HMO and walks out of the hospital unaided three days later. An elderly rabbi, confined to a wheelchair for over a year, spends 20 minutes on Hadassah’s operating table. He, too, leaves within days on his own two feet. A stroke paralyzes the right side of a 42-year-old woman and robs her of speech. Her surgery at Hadassah lasts 14 minutes, and she is discharged later in the week, fully mobile and smiling. An 81-year-old woman from Bethlehem has spent weeks at home, confined to bed by agonizing pain from a fractured spine. Elsewhere, she had been told that her age and heart condition preclude surgery. After an operation at Hadassah, she leaves pain free.
“We treat patients like these every week,” said senior surgeon Dr. Josh Schroeder, director of Hadassah’s spinal deformity unit, who performs around 50 surgeries each month, about half of them using robotics.
Less than two decades ago, no such treatment existed for many of these patients. At HMO today, utilizing robot technology and groundbreaking techniques developed at the medical organization as well as the new $6-million neuro-angiography suite in the Sarah Wetsman Davidson Hospital Tower on Hadassah’s Ein Kerem campus, surgeons are able to minimize risk and perform complex healing techniques.
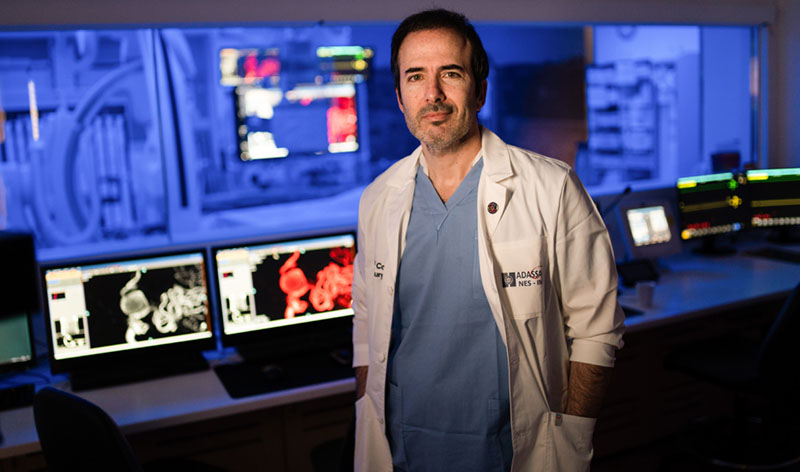
If the word “robot” brings to mind science fiction humanoid killers, it’s time for a reset. “Surgical robots aren’t super-smart, sentient, life-sized dolls,” said neurosurgeon Dr. José Cohen, director of interventional neurology at HMO, its endovascular neurosurgery unit and the neuro-angiography suite—the “mission control” of Hadassah’s robot-assisted brain and spinal surgery, with more than $1 million of its equipment donated by the United States Agency for International Development. “They’re machines with dexterous and sensitive mechanical arms built to manipulate cameras and surgical instruments.” And, he added, “they follow planning software meticulously programmed by surgeons.”
The software that guides the robot minimizes human error and gives surgeons precise real-time control, with the robotic camera transmitting visual information more accurately than the human eye. This means that procedures once considered hazardous can now be performed at minimal risk, and interventions that once required open surgery can be minimally invasive, performed under local anesthetic in less than 20 minutes.

The solution for the 21-year-old man who fell from a ladder and the elderly rabbi in the wheelchair, both of whom asked that their names not be used, was to connect their damaged vertebrae using spinal fusion. “With the robot acting as a kind of GPS, pinpointing the location to the millimeter, and screwing the tiny pedicles [spinal screws] into exactly the right place, we could operate percutaneously”—via minimally invasive needle puncture through the skin—“instead of hours of open surgery followed by weeks of hospitalization,” said Dr. Schroeder.
The shortened time and greater accuracy in using robots means that elderly or ill patients can more easily undergo surgery than in the past. Seventy-three-year-old Lilyah Altschul was brought to Hadassah last summer, able only to move her head because of an infection that caused inflammation and intense pressure on the nerve sac around her spinal column. She had been rejected elsewhere for surgery because of her age and numerous health problems. “One doctor after another gave up on mom,” recalled her daughter, Diana Altschul. Drs. Cohen and Schroeder were able to operate successfully on the septuagenarian using local anesthesia. Just 72 hours after surgery, she was able to walk out of the hospital.
While Hadassah’s spinal surgeons are often able to operate percutaneously, their colleagues who work with endovascular patients must use a longer route. In November 2020, Riki Bitton, a 42-year-old social worker and private investigator living in Moshav Tzalfon in central Israel, woke to find she could not speak or move her right arm or leg. Her husband, Momi Bitton, insisted that the ambulance take them to Hadassah Hospital Ein Kerem.
He suspected a stroke and knew of Hadassah’s specialized cerebrovascular center and stroke unit. Dr. Cohen and his team were scrubbed and waiting. In moments, they cut
a nickel-sized opening in Bitton’s groin and threaded a microcatheter through her vessels to her brain. The images transmitted by the microcatheter’s camera showed a massive blood clot blocking a major cerebral artery. Using a stent retriever to grab and extract the clot, they restored vital blood flow in the brain before permanent damage was done.
“In the 20 years since we opened the endovascular neurosurgery unit, we’ve seen thousands of patients with clots like Riki’s, with narrowed arteries usually because of atherosclerosis, ischemic stroke, aneurysm or brain hemorrhage,” said Dr. Cohen, a global pioneer in the rapidly developing field of robot-assisted neurosurgery. “And they include hundreds of people over 65, who were typically told that their age put them ‘beyond surgery.’ With the huge advances made today, we’re able to perform neurointerventional procedures once considered unacceptably risky.”
Robot-assisted techniques require special expertise. They involve a steep learning curve for surgeons and costly equipment, and are not, therefore, available everywhere. This is evidenced by patients who come to Hadassah from outside the country, including from neighboring nations such as Syria, Lebanon, Iran and Iraq, countries that have no official relationship with Israel. “These patients seek excellence,” said Dr. Cohen, “and our neuro-angiography suite ranks with the world’s best.”
HMO not only embraces new technologies, noted Dr. Schroeder, “it supports their being taken to the next step.”

One such next step was pioneered by Dr. Schroeder himself four years ago, when a 2-ton steel wall fell on 43-year-old factory worker Aaron Schwartz, fracturing six spinal vertebrae and snapping his shinbone, or tibia. “Open surgery would have taken many hours and involved significant blood loss,” said Dr. Schroeder. However, the standard robot-assisted surgery was not the right answer either, because of the patient’s multiple fractures.
The solution that Dr. Schroeder and his team designed was a global first. In a minimally invasive procedure, they positioned an imaging robot, the German-made Siemens Artis Zeego, above the patient to transmit precise real-time, three-dimensional intraoperative images. They then had the Israeli-made Mazor Robotics Renaissance Guidance System insert 11 pedicle screws and connect them to a rod in the spine. It was the safest, most accurate and most automated spinal implant placement performed in the world at that time. Schwartz was able to walk to rehab a couple of days later.
This reconstructive surgery was groundbreaking because it interfaced two different types of robot, explained Dr. Schroeder: “They were made in different countries, according to different technologies and different computer systems. We had to get them to speak the same language and work together.”
Utilizing this combination of technology and disciplines is a major challenge of robot-assisted surgery, but one that Drs. Schroeder and Cohen are confident will continue to be met. “Taking a difficult case, finding a way to treat it and making that treatment the everyday medicine of tomorrow is part of what’s best about being a doctor—and one of the privileges of working in an institution like Hadassah,” said Dr. Schroeder.
“Pushing forward the boundaries of medicine,” added Dr. Cohen, “and sharing what we achieve worldwide, is our moral obligation.”
Wendy Elliman is a British-born science writer who has lived in Israel for more than four decades.










 Facebook
Facebook Instagram
Instagram Twitter
Twitter
Sharon Walker says
Incredible procedures being done! So Brilliant in every way. This is definitely 21st century medicine and hopefully the technology will continue to expand to more surgical procedures. That marrying of the 2 machines for the spinal fusion was Amazing and walk in a few days!
BRAVO Hadassah Drs. and your Teams. Exciting time for medicine.
Margaret Wasserman says
This is truly remarkable – and I say that as an OR nurse with over 35 years’ experience! The expertise, precision, collaboration & teamwork necessary to accomplish feats like these are especially evident at HMO, and the accomplishments deserve worldwide recognition. Congratulations to all involved!