Health + Medicine
Feature
Preserving Fertility After Cancer
Shifra was 28 when she felt a small, hard lump in her right breast. She lay awake through the night before calling her doctor. This was 31 years ago, when breast cancer mortality was a third higher than it is today, but she defeated the disease and considers herself lucky. She accepts that losing her ability to bear children because of the chemotherapy she received was the price for her survival.
Had Shifra—her name has been changed to protect her privacy—been born a generation later, medicine would have had new tools not only to fight her cancer but also to try to preserve her fertility.
“Chemo- and radiotherapies are deadly not only to malignancies but to the ovarian reserve of egg cells or oocytes,” said Dr. Hananel Holzer, associate director of obstetrics and gynecology at the Hadassah-Hebrew University Medical Center and head of two of the department’s sophisticated subspecialties—its units for reproductive endocrinology and infertility (REI) and in vitro fertilization (IVF). With fertility preservation—preserving an individual’s ova, sperm or reproductive tissue—patients can undergo treatment for cancer or other diseases with less fear that such treatment jeopardizes their ability to have children.
“In Israel, some 70 percent of female cancer patients opt for fertility preservation, compared with 50 percent elsewhere in the industrialized world,” Dr. Holzer noted, the difference likely due to “the importance of children in the Jewish faith and culture.”
Hadassah’s oncologists and hematologists routinely refer new patients to the fertility preservation team. Among recent patients is a 22-year-old haredi woman who has just learned that the bulge in her neck is lymphoma. She is married and has a 10-month-old son but wants a larger family. Another is a 40-year-old Muslim woman from East Jerusalem, about to marry for the first time and newly diagnosed with breast cancer. There is also a 34-year-old from outside Jerusalem, whose recently discovered leukemia has halted her high-powered career. She has no partner but hopes one day to marry and have a family.
See related stories: Are You My Surrogate?, The Blessings and Trauma of IVF, Learning to Live My Best Life, Without Children, Hadassah Advocates for Infertility Coverage and Members Share Their Struggles to Become Mothers
They have come to one of the world’s leading fertility preservation specialists. Hadassah-trained, Dr. Holzer was deputy director of Hadassah’s IVF unit in 2001 when it successfully coordinated Israel’s first pregnancy and birth from a cryopreserved (frozen) ovum. Beginning in 2004, he spent 10 years at McGill University Health Centre in Montreal, starting with an REI fellowship and ultimately directing the center’s Gynecologic Reproductive Endocrinology and Infertility Division and establishing its Fertility Preservation Program as well as building a fertility preservation network throughout Canada.

In Israel, Dr. Holzer typically consults with several women every week about preserving their fertility. During a recent visit, the East Jerusalem woman with breast cancer and her fiancée listened attentively and, with Dr. Holzer, decided that a good choice for her was to induce temporary medical menopause with monthly hormone shots. “Making the ovaries less active can reduce the depletion of your egg cells,” Dr. Holzer explained. The hormone has been used for 30 years to treat endometriosis and prevent premature ovulation in IVF. Its success in preserving fertility, however, particularly in breast cancer patients, has only recently been established.
For the young mother with lymphoma whose chemotherapy cocktail must address her entire lymph system, the decision was to harvest ripened eggs from her ovaries before her cancer treatment begins, fertilize them with her husband’s sperm and preserve the embryos. “To harvest mature ova, we once had to wait for the woman’s menstrual cycle to stimulate her ovaries,” said Dr. Holzer. “With today’s methods, we can start ovarian stimulation any time in the cycle. Within nine to 12 days, we’re able to collect the ova, using an ultrasound-guided retrieval procedure.”
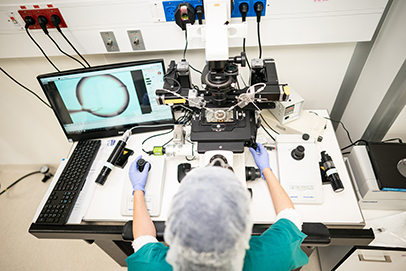
Dr. Tal Imbar, who heads Hadassah’s Fertility Preservation Service, is available 24/7 to harvest ova. As in standard IVF, “we remove as many eggs as we can, fertilize them one at a time in our laboratory and place them in an incubator for about three days,” he said. When the embryos comprise approximately eight cells, they are frozen. Once the lymphoma patient is free of disease, the embryos can be thawed and implanted in her uterus.
The career woman with leukemia decided to preserve her fertility with a variation on this procedure. Not in a committed relationship and unwilling to use donor sperm, she will freeze mature but unfertilized ova—and looks ahead to a healthy future with a partner whose sperm will fertilize her ova in a laboratory using tried and tested IVF techniques.
The use of IVF is one of the underpinnings of fertility preservation, with Hadassah’s expertise in the field among the reasons for the success of its fertility preservation program. Indeed, the IVF clinic at the Hadassah Medical Center in Ein Kerem was expanded last year and a new IVF laboratory was added. A comprehensive new IVF clinic for the hospital’s Mount Scopus campus is currently in the planning stage.
Israel’s hospitals perform some 43,000 cycles a year, with a success rate of slightly more than one in three, on par with leading IVF centers worldwide. Public health insurance funds IVF in women aged 18 to 45 for up to two healthy babies. Further, Health Ministry guidelines permit cryopreservation of ova for all women aged 30 to 41, with use of these ova funded until age 54.
In addition to IVF, Hadassah’s expertise in cryopreservation contributes to its many successful birth stories in patients with fertility problems. “Fertility preservation took a forward leap around 20 years ago when cryopreservation techniques changed, and slow-freezing was replaced by flash-freezing, known as vitrification,” noted Dr. Holzer.
Hadassah’s cryopreservation facility is housed in a former operating suite on the ground floor of the Ein Kerem campus’s Round Building, currently the focus of a renovation fundraising campaign. Entered through sealed double doors and equipped with sensors and alarms and managed by gloved, capped and masked technicians wielding long tongs, the facility’s gleaming tanks fill a vast room. Secured and clearly labeled containers of cells and tissues rest inside the tanks in liquid nitrogen at -320°—the temperature at which all biological processes inside cells cease.

Freeze-thaw survival with vitrification is about 80 percent for ova and 90 percent for embryos, compared with around 60 percent in slow freezing, translating into a difference of thousands of healthy babies.
But what about the pediatric cancer patients who have not reached puberty and do not yet have mature ova to preserve? “We laparoscopically remove a thin layer of ovarian tissue for freezing,” explained Dr. Holzer. “If the ovaries are damaged during treatment, we re-implant this tissue and hope the patient’s oocytes develop into ova.” The first live birth resulting from implanted freeze-thawed ovarian tissue was in Belgium in 2004. The second was in 2005 at Hadassah. In all, some 150 such live births have been reported—an estimated success rate of 30 percent.
For a 9-year-old Hadassah patient about to undergo chemotherapy for Ewing sarcoma, the decision to freeze ovarian tissue was clear-cut to her parents. It was less so for an 11-year-old with Hodgkin lymphoma. Her chemotherapy protocol was likely to be no more than mildly detrimental to her ovarian reserve; her parents nonetheless decided to extract and preserve ovarian tissue.
Today, four years later, her disease has returned, and she is scheduled for an autologous (self-donor) bone marrow transplant. Having come into puberty in the interim—her ovaries survived the earlier treatment—she will now freeze ova prior to the much more aggressive chemotherapy ahead.
Freezing ovarian tissue is currently the only way for pre-pubescent girls to preserve fertility, which puts them ahead of pre-pubescent boys. Testicular stem cells, which produce sperm following puberty, have never been successfully preserved. Working to change that is Swiss-born Dr. Myriam Safrai, 37, a fifth-year Hadassah ob-gyn resident, leading the research under Dr. Imbar, the Fertility Preservation Service head.
“I watched my son fight kidney cancer for four years until his death at age 5, knowing the treatment was destroying his fertility,” Safrai said. “I decided then to find a way to freeze and bank testicular tissue.”
While pre-pubescent boys wait for their solution (adult men have been able to freeze sperm since 1953), the population of women who are looking to preserve their fertility is soaring. What began some two decades ago as an option for cancer patients is now also an answer for women with certain genetic disorders, autoimmune illnesses and endometriosis. It is also embraced by women wanting to postpone motherhood.
There is no one-size-fits-all in fertility preservation, according to Dr. Holzer. Personality, age, relationship status, previous pregnancies, specific disease, planned therapy, urgency of treatment and medications are all part of the decision. There are also no guarantees that fertility preservation will result in a healthy pregnancy. In Israel, he noted, “the live birthrate from implanted ovarian tissue is 30 percent. That from embryos is 40 to 50 percent until age 35, and then declines. From frozen oocytes, the live birthrate is around 40 percent until age 35, and declines thereafter.” These rates are equivalent to successful fertility preservation centers worldwide.
“Sometimes patients are too overwhelmed by their diagnosis to think about preserving their fertility, so alternatives such as ova donation, surrogacy and taking no action are among those we present to them,” said Dr. Holzer.
Diagnosis of malignant disease is inevitably a crisis, he said, “but as patients prepare to fight life-threatening illness, preserving their future fertility from the therapies is critical.
We provide options to do so—together with hope—to help them in their struggle against their disease.”
Wendy Elliman is a British-born science writer who has lived in Israel for more than four decades.
The Online Hadassah Magazine Discussion Group presents “Struggling With Infertility,” an exclusive live web interview with Amy Klein, author of The Trying Game: Get Through Fertility Treatment and Get Pregnant Without Losing Your Mind, moderated by Lisa Hostein, executive editor of Hadassah Magazine. Register here and receive a link to watch the interview on your computer or mobile phone.









 Facebook
Facebook Instagram
Instagram Twitter
Twitter
Leave a Reply